Breast reduction or reduction mammaplasty surgery is one of the most satisfying procedures for women with excessively large breasts who complain of neck, shoulder, or back pain.
When large breasts interfere with a woman’s quality of life, this procedure may be covered by your insurance company if certain criteria are met.
Patients who undergo breast reductions are among the happiest of all plastic surgery patients.
The consultation
As both a woman and a plastic surgeon, Dr. Parcells is distinctively qualified to address your concerns and tailor her technique to achieve your desired results.
During the consultation, Dr. Parcells will discuss your medical history and family history of breast disease. She’ll ask you about your current concerns and desired goals including breast size and shape.
She’ll then complete a physical exam and a member of her team will take non-identifiable medical photographs of your breasts (without your face) for your chart and for surgical planning.
How to prepare for surgery
You need to be in good physical shape to ensure proper healing, so follow your surgeon's instructions before and after breast reduction surgery.
Before you undergo surgery, Dr. Parcells will need to review the results of your routine mammogram if you are older than 40. Certain medications and herbal supplements will need to be stopped to reduce the risk of bleeding.
Additionally, if you require any medical or hematological clearances those will be received prior to your surgery. All women with a history of smoking cigarettes, marijuana, or vaping will be asked to refrain 8 weeks before and after surgery and be tested prior to your surgery.
The breast reduction procedure itself
For most women, breast reduction surgery is often performed in an outpatient surgical center. You will receive general anesthesia and in the recovery room an anesthesiologist will administer a pain block to alleviate breast discomfort.
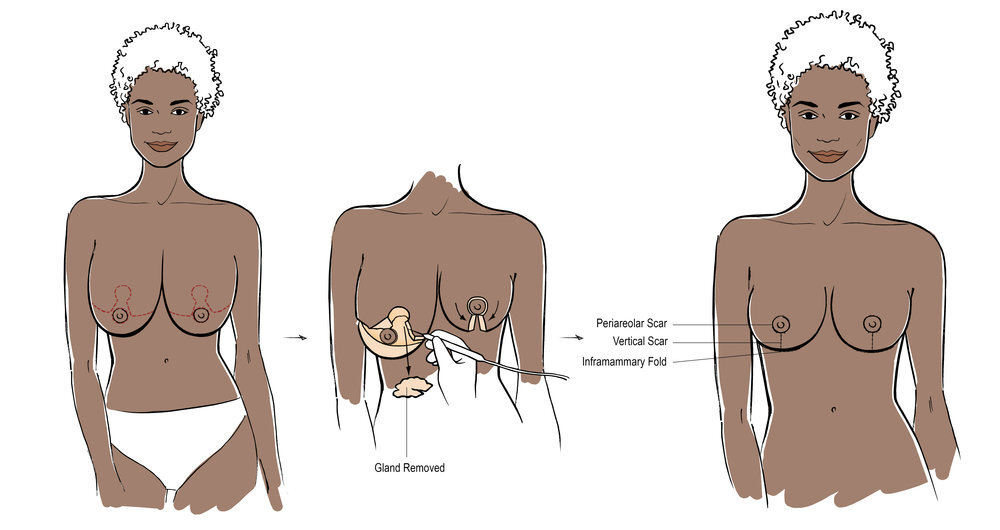
Dr. Parcells will focus on removing excessive skin and breast tissue and reshaping your breasts into a more youthful shape. Depending on your prior discussion, liposuction of the breasts may be performed in conjunction with the excision of breast tissue to further define your silhouette.
Depending on how much breast tissue is removed, drains may be placed and they will be removed in the office. You will be wrapped up in a surgical bra and gauze after your procedure.
Your Immediate Recovery
Most women experience mild to moderate discomfort for several days following surgery and are back to their activities of daily living by about a week. Most patients experience immediate relief of back, shoulder, and neck pain with their new, smaller breasts.
You will see Dr. Parcells in the office the following day and your breasts will be examined. If drains are in place, they are usually removed a few days after surgery.
To ensure a healthy and straightforward recovery, it’s important to eat a healthy, high-protein diet, with small meals throughout the day.
It is normal to feel tired and you should be encouraged to receive plenty of rest.
Frequent small walks during the day are helpful in improving circulation, but vigorous exercise or heavy lifting is highly discouraged as your incisions (stitches) could pop open into wounds.
Most patients are off pain medications by 3-5 days and are able to drive once they are off narcotics for 24 hours.
Antibiotics are administered up to 5 days after surgery.
Most women return to work or school in about 5 days – 1 week.
Any stitches that are placed are removed 1-4 weeks after the procedure, depending on their location.
Physical activity at the gym can resume around 4-6 weeks after surgery. Patients are in special surgical bras to assist in shaping for several weeks after the procedure.
Your new breasts may feel firmer and look rounder. Breast reduction may change the normal feeling in your breast. But in time, some feeling may return.
Breast Scarring
Scars are required in order to reduce the size and reshape your large breasts. These scars are usually located around your nipple, down the bottom of your breasts and underneath your breasts. These scars are not noticeable while wearing a bra and most bathing suits. The majority of the time, the scars will fade over time, but will never completely disappear.
To learn more about a breast reduction, or to schedule a consultation with Dr. Parcells, please visit her website.
Dr. Parcells is a board-certified plastic surgeon specializing in breast reconstruction and aesthetics. She is a member of The Aesthetic Society and a candidate member of the American Society of Plastic Surgeons.