Breast augmentation is one of the most common cosmetic surgeries performed in the United States every year. Women typically desire this procedure to improve their breast size and shape.
What is breast augmentation?
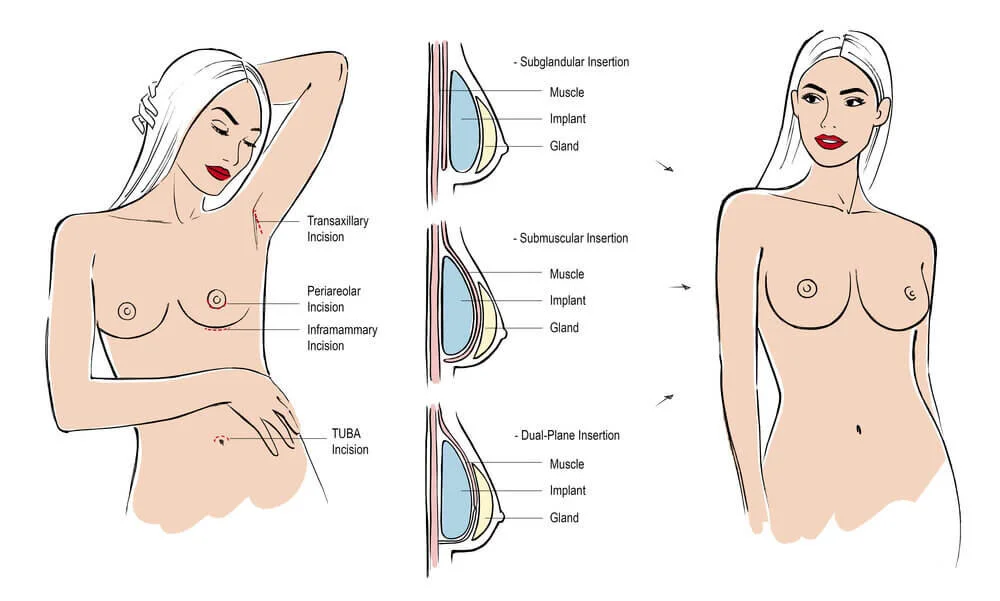
There is a lot to understand about the type of breast implants (silicone or saline), where they are placed (above or under the muscle), placement of scars.
Additionally, a breast augmentation can be combined with a breast lift or mastopexy. This surgery changes the shape of your breasts, but it doesn’t alter the size.
How to find a surgeon
The most important part of considering breast augmentation is choosing the right surgeon. Make sure you see a board-certified plastic surgeon.
Ask questions about your procedure and make sure you feel comfortable with your surgeon of choice
Surgeons website to find a board-certified plastic surgeon near you.
And while preoperative planning is important to optimize your surgery, recovery is just as essential to ensure an excellent outcome.
How long is a full recovery?
In general, full recovery from a breast augmentation can take on average 6 weeks. Each person is different, so for specifics make sure you talk to your board-certified plastic surgeon.
Let’s break down the recovery into a few stages so you can better understand how to prepare.
Acute Recovery:
This period is usually immediately post-operation.
Your breast will be wrapped and you will be transported to the recovery room, where you will likely feel groggy and sore.
At this point, your surgeon may elect to give you a local numbing pain block to improve any discomfort you are experiencing and reduce narcotic use. This typically lasts around 12 hours.
Because you have just woken up from anesthesia, you will need someone to drive you home and stay with you overnight.
The first 3 to 5 days
The first few days after surgery are the most uncomfortable.
Your surgeon will recommend instructions on how often to take antibiotics and muscle relaxants or pain medications for the first few days after your procedure.
Ideally, any strong narcotic medications should be discontinued within the first few days since they cause constipation and prolonged use can lead to a longer recovery.
While some patients report pain, most patients experience tightness or muscle aching at this time.
This can be in the breasts, shoulders, neck, and back. These symptoms are best controlled with a muscle relaxant such as Valium. For most women, this sensation resolves over the next 3 to 5 days.
You will also have instructions on how to care for your incision and what bra or garments to wear.
Bruising, swelling, and minor bleeding from the site is all normal. If something does not feel right, call your doctor.
1 week
By this time, you should have minimal discomfort that can be managed with over-the-counter medications.
You should be seen by your surgeon within this time frame, and most women are able to resume light daily activities. Women who work at desk jobs are usually fine to return to work and drive. Many physicians encourage a few short walks 1-2 times a day.
Next few weeks
During this time, you will start to feel like yourself again and get back into your routine.
It’s important to note that your wound heals approximately 10% per week and so most doctors do not recommend resuming an exercise routine, especially upper extremity focused workouts, until about 4-6 weeks after surgery.
Additionally, patients with labor-intensive jobs may have to wait 3-4 weeks after their procedure before returning.
If you have a physically demanding job, you’ll need to be out of work for 3 weeks or more. You’ll also need to avoid heavy lifting and intense physical activities, like running.
2 months
After about 2 months, your physician should assess your healing and clear you for all normal activities.
It's vital to follow your doctor's care instructions closely so that your breast implants heal properly and there are no complications.
Possible complications
Breast augmentation is a surgical procedure, and every procedure has potential risks. Complications can include
Unsightly scars
infections
bleeding problems, like blood loss.
Asymmetries between your breasts
Implant malposition
Breast and nipple pain or numbness
Poor cosmetic result
breasts appear to merge (symmastia)
skin dimpling or visibility of the implant
scarring around the implant
implant leak or break
Tips for recovery
There are things you can do in order to avoid complications and enhance your recovery experience.
Make sure you discuss all concerns with your physician before the surgery.
Follow instructions regarding medication frequency and duration, wear your surgical garments as instructed, and avoid activities that your physician discourages.
Ask friends and family to help. Prepare healthy meals ahead of time and take the rest you need to heal well.